Sometimes men are faced with such an unpleasant ailment as bacterial prostatitis. To start treatment in time, it is important to know by what signs the disease can be determined and what diagnoses and therapies will be needed.
Bacterial prostatitis is an infectious disease of the prostate gland. Symptoms of the disease include pain in the perineum, increased body temperature, body intoxication and other signs. Such a condition may require emergency hospital admission, as it can pose a threat to the patient's health and life.
Forms of bacterial prostatitis
Depending on the course and the symptoms manifested, bacterial prostatitis is divided into two forms: acute and chronic.
Sharp
The acute form occurs unexpectedly and is accompanied by various unpleasant symptoms. The acute form of bacterial prostatitis requires immediate medical attention. This pathological process is provoked by Escherichia coli, staphylococci, enterobacteria.
Acute prostatitis is easily diagnosed using laboratory tests. Severe symptoms and clinical picture allow for an accurate diagnosis. Treat this form of prostatitis in a complex way using drugs and physiotherapy.
chronic
Chronic bacterial prostatitis has a pathogenic pathogen that can be determined using laboratory tests and studies. The main pathogens are gonococci, chlamydia, ureaplasma, mycoplasma. The inflammatory process can also be caused by tuberculosis bacteria or fungi of the genus Candida, if the man has HIV infection.
Types of bacterial prostatitis
Bacterial prostatitis is classified according to the type of pathogen:
- tuberculous (Koch's bacillus);
- gonorrhea (gonococci);
- fungal (various types of fungi);
- chlamydia (chlamydia);
- viral (causative agents of herpes, human papillomavirus, flu);
- mixed (several different infections).
It is possible to determine exactly what the causative agent was only under laboratory conditions, since the symptoms are the same for everyone.
Causes and risk factors
Bacteria enter the prostate gland, causing acute or chronic prostatitis. Sexually transmitted diseases can also cause this disease. In some cases, the cause cannot be determined.
causative agentsbacterial prostatitis are considered:
- colibacillus;
- klebsiella;
- proteus;
- fecal enterococcus;
- Pseudomonas aeruginosa.
Possiblemicrobiological reasonsprostatitis are:
- staphylococci (saprophytic, golden, epidermal);
- genital mycoplasma;
- chlamydia trachomatis;
- ureaplasma;
- Trichomonas.
TOrisk factorsinfection of the prostate gland with the subsequent development of the inflammatory process in the form of one or another form of bacterial prostatitis are:
- intraprostatic reflux (reflux of urine into the ducts of the prostate gland when urinating);
- pelvic injury;
- unprotected anal sex;
- urinary tract infections;
- have an indwelling urethral catheter or intermittent bladder catheterization;
- transurethral diagnostic and therapeutic interventions;
- HIV-AIDS;
- previous prostate biopsy.
Bacterial Prostatitis Symptoms
Usually, with bacterial prostatitis, the symptoms are so pronounced that it is difficult not to pay attention to them. Signs of the disease include:
- high body temperature (in the anus it is usually higher than in the armpits);
- fever and chills;
- difficult and painful urination, especially at night;
- possible development of constipation due to an enlarged prostate gland;
- pain in the lower body (lumbar, perineum, lower abdomen);
- general intoxication of the body;
- discharge from the urethra and blood in the semen.

Stages of bacterial prostatitis
The clinical picture of bacterial prostatitis manifests itself depending on the stage of the disease and the degree of involvement of the prostate tissue in the inflammatory process. Share:
- Primary or catarrhal prostatitis.It is characterized by inflammation of the walls of the prostate gland. It is quite possible to cure it with antibiotics in 10 days.
- Secondary or follicular.It is characterized by the formation of abscesses in the glandular tissue. It is accompanied by a high fever. This form is also effectively treated with antibacterial drugs.
- Tertiary or parenchymal.The pathological process at this stage extends to the entire organ: the prostate increases in size, swells and changes shape. If you don't take timely treatment, the tertiary stage can turn into chronic prostatitis.
Possible complications and consequences for men
The consequences and complications of bacterial prostatitis include:
- vesiculitis (inflammation of the seminal vesicles) - manifested by pain in the groin, premature ejaculation, painful erection;
- colliculitis (inflammation of the seminal tubercle) - differs in various symptoms - burning and tickling of the posterior urethra, painful sensations during orgasm, blood in the sperm;
- violation of potency;
- prostate sclerosis;
- infertility;
- prostate cyst;
- abscess of the prostate;
- stones in the prostate gland.
Chronic pelvic pain syndrome is one of the most serious consequences of chronic prostatitis.
Asymptomatic inflammation is the mildest form in terms of no complaints. This type of prostatitis is diagnosed with the development of complications of the reproductive function.
Is bacterial prostatitis dangerous for women?
Prostatitis in women does not occur, but its serious consequences are common. If a man is suffering from bacterial prostatitis, it is simply irresponsible to say that a woman is not in danger: chlamydia, ureaplasma, Trichomonas, mycoplasma, gonococcus, gardnerella and other infections received by her from a partner pose a serious danger to a woman and bring to the development of various gynecological diseases.
Which doctor is he treating?
Urologistis considered the leading specialist who deals with the diagnosis and treatment of pathological conditions of the genitourinary system.
Andrologist.Despite the fact that andrology belongs to a fairly young branch of medicine, specialists in this area are gradually taking their place in the treatment of diseases of the male genitourinary system. The advantage of this doctor is his narrow focus. Unlike a urologist who treats diseases of the male and female genitourinary tract, the andrologist specializes exclusively in male problems.
Bacterial Prostatitis Diagnosis
If bacterial prostatitis is suspected, numerous tests are done, including:
- scrapings and swabs for infection;
- cultures for flora and antibiotic sensitivity;
- a general blood test helps to detect the inflammatory process, when there is an increase in the number of leukocytes, an increase in ESR;
- spermogram, which examines a decrease in the number of spermatozoa, a violation of their mobility;
- three-glass urine sample (studies inflammatory changes in the urine);
- general urine analysis;
- analysis of prostate secretion;
- uroflowmetry - observation of the daily amount of urine.
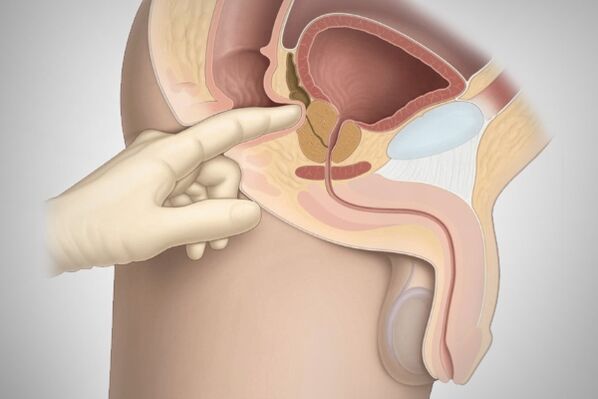
The doctor will be able to assess how enlarged the prostate is by a digital rectal exam. To clarify the diagnosis, your doctor may refer you to a transrectal ultrasound.
Treatment of bacterial prostatitis
As a therapy for bacterial prostatitis, drugs, physiotherapy, folk remedies and, in severe cases, surgery are prescribed.
Pharmacological treatment
Medical treatment of prostatitis is carried out using various groups of drugs. These can be antibiotics to neutralize the pathogen. However, they do not always help, as the prostate gland is characterized by poor absorption of antibiotics from the protected penicillin group, fluoroquinolones.
The course of treatment is usually 10-14 days and must be completed without fail, since if bacterial prostatitis is not treated, it will reappear. Vitamins and drugs are also prescribed to strengthen the immune system.

Surgical intervention
The doctor proposes surgery for prostatitis if no results have been achieved in treating a patient with medications, physiotherapy, or alternative treatment methods.
Surgery includes the following procedures:
- Transurethral resection of the prostate.The internal part of the organ is removed. Surgery is the most commonly used and best endoscopic treatment for benign prostatic hyperplasia.
To perform this surgery, the patient performs a series of tests, including blood and urine tests. The operation is performed under spinal anesthesia, but general anesthesia can also be used. There are no scars after the operation. Among the disadvantages is painful urination in the first days after the procedure. - Laser surgery.The laser destroys the diseased tissue. At the same time, the size of the prostate decreases and the vessels are "sealed" and do not bleed. The operation is performed without incisions, and the postoperative period is only three days. Before surgery, blood and urine tests are performed, as well as ultrasound of the urinary tract and, as prescribed by the doctor, a prostate biopsy is performed.
This method is not effective if the prostate volume is large. - Open prostatectomy.The operation is performed in cases where the prostate is very enlarged, in the presence of complications and in case of damage to the bladder.
The surgeon makes an incision in the lower abdomen or between the scrotum and anus. Part of the prostate is removed or is completely.
Before the operation, ultrasound, MRI, and cytoscopy are performed, as well as blood and urine tests and a prostate-specific antigen test.
One of the advantages of the operation is its effectiveness in treating the prostate and related problems. And from the minuses: a long postoperative recovery period (more than a month), as well as problems with erectile function. - Transurethral incision of the prostate gland.The doctor does not remove the prostate tissue, but only makes an incision to relieve pressure on the urethra, thus making urination easier. Before the operation, blood and urine tests are performed, as well as an ultrasound of the urinary tract.
Advantages of the procedure: Prostatitis symptoms are relieved without the risk of retrograde ejaculation, long-term recovery is not required. Among the shortcomings, prostatitis has yet to be treated. - Prostate abscess drainage.The doctor opens the abscess through the perineum or rectum, dissecting the skin and subcutaneous tissue and introducing a drain into the cavity with pus for removal.
Before the operation, a consultation with a proctologist is performed, blood and urine tests are carried out.
The advantages of the operation include the absence of the risk of loss of sexual functions. The disadvantages are that the abscess may not be completely removed and bacteria can spread throughout the body.
Prostatitis surgery in men is usually a last resort for chronic bacterial prostatitis associated with complications of any form.
Physiotherapy
In the complex treatment of patients diagnosed with prostatitis, physical methods of influence are of great importance. As a result of physiotherapy procedures, they have improved:
- Blood flow;
- lymphatic drainage, which contributes to the elimination of decomposition products of microorganisms;
- blood and lymphatic circulation, due to which inflammatory infiltrates resolve;
- outflow of blood and lymph, which helps reduce congestion in the pelvis;
- metabolism;
- activity of cell membranes, which promotes the penetration of active drugs into the cell.
Physiotherapy for bacterial prostatitis includes the following methods:
- Electrophoresis.Impact on the body with ions, which helps relieve inflammation and eliminate pain.
- Laser physiotherapy.The laser helps relieve perineal pain and improves blood flow to the pelvic organs. It kills bacteria and removes the waste products of harmful organisms.
- Magnetotherapy.When carrying out this procedure, the permeability of tissues improves, and the effectiveness of drug therapy increases significantly. Also, with the help of magnetotherapy, hemodynamics and congestion are stopped.
Exercise for bacterial prostatitis
Exercise for chronic prostatitis causes the muscles in the pelvic region to contract, which ensures a difference in intra-abdominal pressure. This promotes blood flow to the prostate. Exercise tones the nervous system, makes the adrenal glands work and removes the residual effects of inflammatory diseases in the prostate.
You can do the following exercises at home:
- The man sits on a rubber ball and rolls from left to right, jumping slightly. He helps strengthen the pelvic floor muscles and the obliques.
- Kegel exercises. For 5-10 seconds, he strains his buttocks as much as possible, then relaxes the muscles. This exercise is performed 20-50 times.
- Lie on your back, he bends your knees and rests your heels on the floor. He slowly raises his pelvis while keeping his upper back flat on the floor. When the pelvis is at its highest point, you need to freeze for 15 seconds, then return to its original position. The number of repetitions is 10-15 times.
Perform a massage
To achieve the result, exercises are performed every day, and are also supplemented with prostate massage, which can be performed both independently and with the help of special massagers.
Self-massage of the prostate is performed as follows:
- Drink a liter of water one hour before the procedure to fill the bladder.
- Cleanse the intestines with an enema based on a solution of potassium permanganate or chamomile infusion. The horse needs to be rinsed.
- Hands should be washed thoroughly and nails cut short.
- It is necessary to wear a glove or condom on the finger that will be used for the massage.
- The rubber surface of the protective layer is lubricated with petroleum jelly, grease or baby cream.
- Lie down in a comfortable position and insert your finger into the anus to a depth of 5 cm.
- On the front wall, you can feel the prostate gland and start stimulating it with light strokes from the sides to the center.
- On hard areas, the pressure is gradually increased, and on soft areas it is reduced.
- In the final stage, stroking movements are performed downward along the central groove.
- Gently pull your finger out of the anus.
During the massage 3-5 drops of liquid (prostate juice) should be released. Immediately after the massage, you need to go to the bathroom and empty your bladder.
Diet therapy
With prostatitis, it is necessary to reduce the use of alcohol and cigarettes as much as possible. In addition, doctors recommend excluding from the diet:
- fatty foods, especially meat, since fat is a source of "bad" cholesterol, which disrupts blood circulation and adversely affects the prostate;
- energy and synthetic drinks;
- spices;
- spicy and smoky.
It is recommended to eat boiled and steamed foods, a lot of vegetables and herbs.
Folk remedies
Pumpkin seeds.Pumpkin seeds are an ancient remedy for prostatitis. They contain a lot of zinc, which the male body needs. You need to eat 30 seeds a day before meals.
Hazel branches.Boil a few sprigs of hazelnut with leaves in water for 20 minutes, leave to infuse until the broth takes on a red-brown color. A weekly course is enough for a cure.
Poplar bark.Poplar bark must be harvested at the beginning of the sap flow period, before the buds bloom. We are about the second half of April. Dry the bark in the oven, take 100 g, grind and put in a half-liter jar. Pour 200 g of vodka so that the bark is completely covered. Close the jar and put it in a dark place for 2 weeks. Filter after 2 weeks. Take 1 teaspoon in three three-week courses with a 10-day break.
Prognosis for bacterial prostatitis
The prognosis for bacterial prostatitis depends on the stage and type of the disease. The duration of the disease also affects the prognosis: the longer the inflammation is maintained, the longer it takes to treat the complications of prostatitis.
In acute prostatitis, the prognosis is favorable. Chronic bacterial prostatitis is often a recurrent form, even when conservative therapy is prescribed. With long-term treatment of the chronic form, changes in potency may occur.
Prevention measures
Prevention of bacterial prostatitis can be divided into primary and secondary.
Primary prevention of prostatitis:
- a healthy lifestyle;
- Proper nutrition;
- Playing sports.
Preventive measures at home are important - performing exercises that activate blood flow in problematic organs and improve muscle tone.
Also, men should study Kegel exercises. They were developed for postpartum recovery in women, but are used to train a man's anal muscles and rectum.
Gymnastic exercises are useful: bicycle, birch, bridge, candles. They train the pelvic muscles. It is recommended to perform leg swings, apnea exercises and take a contrast shower.
Secondary prevention of prostatitis:
- Pharmacological treatment;
- regular examination by a urologist, regardless of the manifestations;
- within a year of treatment, undergo quarterly examinations, thereafter - once every six months.
For secondary prevention, rectal suppositories are used. They work through the rectum. Usually, these drugs have few contraindications. Also, to prevent the recurrence of bacterial prostatitis, biologically active drugs are prescribed.
The earlier prostatitis is detected, the easier it is to cure it. Therefore, do not neglect regular visits to the doctor. After the diagnosis, the doctor will select the appropriate drugs and prescribe a therapeutic course. If the disease progresses, taking medications quickly relieves symptoms and helps you stay active and functional.
































